The CDC Has Bad News If A COVID-19 Antibody Test Made You Think You Had Immunity
COVID-19 serologic tests that aim to identify whether people have already come into contact with coronavirus could be giving false hope, the CDC has warned, cautioning that false-positives are likely in many situations. Currently, two types of COVID-19 testing are primarily underway as the extent of the pandemic is measured, focusing either on whether patients are currently infected with the virus, or whether they have been in the past.
Both are important factors to track. Viral tests look for whether someone is currently infected, and were the first to be deployed as governments attempted – with different rates of urgency – to measure how much community spread the disease was demonstrating.
Antibody tests, also known as serological tests, don't show whether a patient is currently infected, but do attempt to flag whether they previously had coronavirus. They rely on the presence of antibodies – the immune system's response to infection – in the body. However those can take 1-3 weeks to be produced, and it's still unclear whether exposure to COVID-19 and subsequent recovery automatically means someone can't be re-infected later on.

Still, both types of testing is underway, taking advantage of the FDA's Emergency Use Authorization for non-approved diagnostics deployed during a time of pandemic. We've already seen warnings from the FDA about manufacturers of serology tests over-stating the potential benefits of their products, and tougher rules from the agency about how those types of tests are implemented. Now, the Centers for Disease Control are adding their own note of caution.
In COVID-19 testing there are false-positives and false-negatives
No test is perfect. False-positives are when a test says you have a disease or infection, but in reality you don't. False-negatives are the opposite: you are, in fact, infected, but the test says you're not.
Both can be problematic in their own ways. If you get a false-negative result for COVID-19 in a viral test, you could assume you're not infected and thus go about inadvertently passing it to other people. That's all the more likely, considering some people are asymptomatic, and as such don't show outward signs that they're infected with coronavirus.
For serological tests, false-positives are arguably more dangerous, since they can lead to a misguided sense of security. For a start, there's no guarantee that, having once been infected with COVID-19, you're protected from future infections. The limitations of the tests themselves, the CDC has warned this week, also pay a significant role.

In updated guidance, the CDC flagged that false-positives are likely "in most of the country" right now, "including areas that have been heavily impacted" by COVID-19. That's because the accuracy depends on how many people in the population overall have been infected and thus developed antibodies.
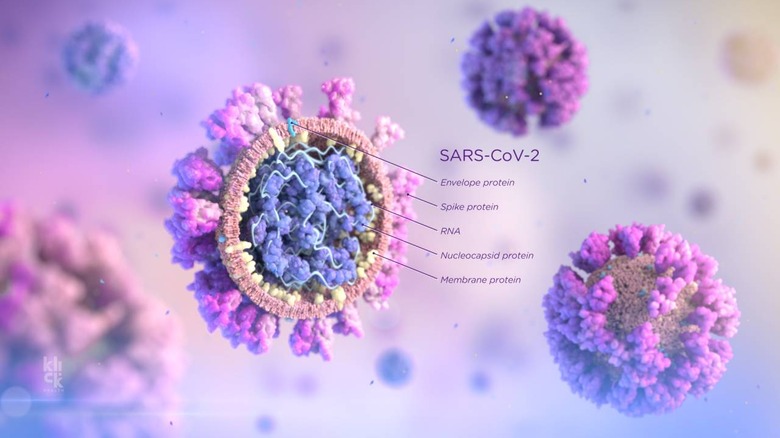
Even in those heavily-impacted areas, the CDC suggests, the SARS-CoV 2 antibody is likely to be of low prevalence, anything from 25-percent at most or under 5-percent at the low end. In that case, "testing at this point might result in relatively more false positive results and fewer false-negative results," the agency cautions.
"For example, in a population where the prevalence is 5%, a test with 90% sensitivity and 95% specificity will yield a positive predictive value of 49%," the CDC explains. "In other words, less than half of those testing positive will truly have antibodies. Alternatively, the same test in a population with an antibody prevalence exceeding 52% will yield a positive predictive greater than 95%, meaning that less than one in 20 people testing positive will have a false positive test result."
There are workarounds for COVID-19 tests, but nothing is perfect
The best strategy, the CDC says, is to continue testing but be mindful of its limitations. If a positive result from a serological test is given, then it's best to follow that up with a second, different test to be sure it's not a false-positive. That's known as orthogonal testing.
Even if both tests show up positive, that isn't an automatic guarantee of safety from future coronavirus infection. We won't know how that works until further research into the durability and duration of any immunity is completed.
"Asymptomatic persons who test positive by serologic testing and who are without recent history of a COVID-19 compatible illness have a low likelihood of active infection and should follow general recommendations to prevent infection with SARS-CoV-2 and otherwise continue with normal activities, including work," the CDC suggests.
Still, serologic test results shouldn't be the measure by which returning people to the workforce are made, the CDC says, and nor should they be used for decisions about grouping people. That includes schools, dormitories, jails, and other settings like churches.
